What Patients Need to Know – Breast Cancer & Fertility Preservation – Timing of Egg Harvest

The number of women diagnosed with breast cancer within their reproductive years is growing. Chemotherapy for breast cancer can have an adverse effect on a woman’s ability to have children.
Fertility preservation means preserving the ability of a woman or a couple to start a family at a time of their choosing. For most cancers, posttreatment pregnancy does not increase the risk of cancer progression or obstetric or neonatal complications. Improvement in cancer treatment management and increasing survival rates has therefore created an increased need for fertility preservation.
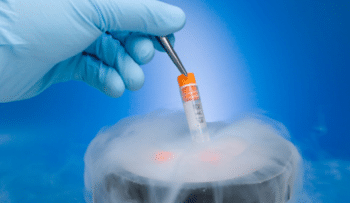
Oocyte and embryo cryopreservation are now well-established techniques for preserving fertility, but they have their limitations. Both chemotherapy and radiotherapy have a major impact on reproductive potential and fertility preservation procedures should be carried out prior to these treatments. The impact of chemotherapy drugs on the ovary is variable ranging from no effect to complete ovarian atrophy. The degree of damage is dependent upon the type of the chemotherapeutic drug, the dose, the patient’s age and ovarian reserve. Older women have a lower ovarian reserve and hence are more susceptible ovarian damage, premature menopause and varying degree of infertility.
The American Society of Clinical Oncology first published recommendations on fertility preservation in 2006 and stated that patients treated during their reproductive years should be informed about fertility preservation options and referred to reproductive specialists.
Fertility preservation techniques for woman typically include: Embryo cryopreservation or Oocyte cryopreservation
Embryo cryopreservation – requires a woman go through IVF. The harvested egg is fertilized with sperm and the embryo is then frozen or cryopreserved for later use. A sperm sample from a partner or a donor is required for oocyte fertilization. This is a well established technology that provides a good success rate depending on the number and quality of embryos stored. A live birth rate of 38.7% per embryo transfer is reported for frozen embryo transfer.
Oocyte (egg) cryopreservation – Allows for the freezing of eggs that have not been fertilized for a woman who does not have a partner or sperm donor. Oocyte preservation avoids the religious or ethical questions of unused embryos and also allows a women to maintain reproductive autonomy. Oocyte cryopreservation also requires the patient to go through ovarian stimulation and egg retrieval. Pregnancy and live birth rates from oocyte cryopreservation have improved considerably.
Downside and Risks:
- Stimulation of estrogen-sensitive (ER+) breast cancer is a risk for patients undergoing ovarian stimulation. Anti-estrogen medications letrozole and tamoxifen can be added to lower estradiol levels in patients with these tumors.
- Other risks include ovarian hyperstimulation syndrome and blood clots or thromboembolism.
- In order not to delay cancer treatment only one attempt at embryo or oocyte cryopreservation can typically be performed with only a limited number of oocytes/embryos collected. This limits the number of future pregnancy attempts.
Ovarian tissue cryopreservation – is an experimental technique that involves surgically harvesting ovarian tissue and freezing the tissue. The tissue is later re-implanted after completion of cancer therapy. When successful, ovarian function resumes in a few months. If transplanted back into the pelvis spontaneous pregnancy can occur but IVF is often necessary if the tissue is not in the pelvis. This technique has future potential advantages in that it does not delay the start of cancer therapy, avoids the risk of ovarian stimulation and there is no need for a partner or donor sperm. It preserves a larger number of follicles and allows for ovarian function.
Timing of fertility preservation in breast cancer:
- Fertility preservation consultation should be arranged at the time of initial diagnosis.
- The best time for fertility preservation is after surgery and before adjuvant therapy.
- Ovarian stimulation takes approximately 2 weeks from the 2nd day of the period and therefore must be coordinated and planned so as not to delay cancer treatment.
- New methods of ovarian stimulation such as ‘luteal phase stimulation’ and ‘random start protocols’ can be used to overcome time constraints and avoid waiting for the menstrual cycle.
- For woman who are BRCA+ or other genetic risks who wish to undergo fertility preservation prior to elective ovary removal, these options as well as others that have fewer time constraints are available.
For more information: visit https://www.reproductivefacts.org/faqs/frequently-asked-questions/ or search ASRM and fertility preservation.